Part D. Chapter 2: Dietary Patterns, Foods and Nutrients, and Health Outcomes
What is the relationship between dietary patterns and risk of type 2 diabetes?
Conclusion Statement: Moderate evidence indicates that healthy dietary patterns higher in vegetables, fruits, and whole grains and lower in red and processed meats, high-fat dairy products, refined grains, and sweets/sugar-sweetened beverages reduce the risk of developing type 2 diabetes.
DGAC Grade: Moderate
Evidence is lacking for the pediatric population.
Review of Evidence
The Committee considered two sources of evidence. The primary source was the NEL Dietary Patterns Systematic Review Project which included 37 studies predominantly of prospective cohorts design and some randomized trials (n=8).1 This primary source was supplemented by a published meta-analysis that included 15 cohort studies of which 13 overlapped with the NEL review.2 The meta-analysis provided an estimate of the effect size of incident type 2 diabetes associated with a healthy and unhealthy dietary pattern.
Although the NEL rated the overall body of evidence for type 2 diabetes as limited, this was primarily a result of examining the different methods for defining dietary patterns (e.g. indices, data driven, and reduce rank regression) separately. As such, the NEL noted these methodological inconsistencies across studies but stated general support for the consumption of a dietary pattern rich in vegetables and fruits and low in high-fat dairy and meats. The DGAC concurred with this conclusion. However, the DGAC has elevated the grade of the entire body of evidence to moderate given that the NEL findings were corroborated by the results of a high quality meta-analysis (AMSTAR rating of 11) and the magnitude of the associations that showed when the results of 15 cohort studies are pooled, evidence indicated a 21 percent reduction in the risk of developing type 2 diabetes associated with dietary patterns characterized by high consumption of whole grains, vegetables, and fruit. Conversely, a 44 percent increased risk of developing type 2 diabetes was seen with an unhealthy dietary pattern characterized by higher consumption of red or processed meats, high-fat dairy, refined grains, and sweets.
Dietary Patterns and Incident Type 2 Diabetes
Dietary Approaches to Stop Hypertension (DASH)
One study used the DASH score in a cohort of 820 U.S. adults ages 40 to 69 years and with equal sex distribution and racial diversity.3 Liese et al. found adherence to the DASH score was associated with markedly reduced odds of type 2 diabetes in Whites but not in the total population, or in the Blacks and Hispanics, which comprised the majority of this cohort.
Mediterranean-style Dietary Patterns
Three studies assessed Mediterranean-style dietary pattern adherence (Mediterranean Diet Score [MDS]) with sample sizes ranging from 5,000 to more than 20,000 in both Mediterranean and U.S. populations. One study conducted in Spain with the SUN cohort (n=13,380) found a favorable association between the MDS (the original MDS of Trichopoulou) and risk of type 2 diabetes. Overall, a 2-point increase in MDS was associated with a 35 percent reduction in risk of type 2 diabetes.4 Another study, conducted in Greece with the EPIC-Greece cohort (n=22,295), also assessed the relationship between the MDS and type 2 diabetes. In this second Mediterranean population, adherence to the MDS also was favorably associated with decreased risk of diabetes.5 Conversely, a study conducted in the United States, using the authors’ MedDiet Score with the Multi-Ethnic Study of Atherosclerosis (MESA) cohort (n=5,390) found no association between their MedDiet Score and type 2 diabetes incidence in the total population, in men or women, or in specific racial/ethnic groups.6
Dietary Indices based on the Dietary Guidelines
Four studies used dietary-guidelines based indices such as the AHEI and the Diet Quality Index (DQI). The sample sizes of the studies ranged from 1,821 to 80,029. A study that assessed adherence to the AHEI in the United States found a favorable association between AHEI score and risk of incident type 2 diabetes in women in the Nurses’ Health Study (n=80,029).7 In the CARDIA study (n=4,381), also from the United States, the authors found no association between DQI-2005 score and type 2 diabetes incidence in the total population or in Blacks or Whites.8 Studies from outside the United States included one conducted in Australia using a Total Diet score in the Blue Mountains Eye Study (BMES, n=1,821) and one from Germany using a German Food Pyramid Index with the EPIC-Potsdam cohort (n=23,531). Neither found an association between these scores and incident type 2 diabetes.9, 10 Thus, evidence for an association only exists with the AHEI, which does contain slightly different components from the other indices, such as nuts and legumes, trans fat, EPA + DHA (n–3 FAs), PUFAs, alcohol, red and processed meat.
Data-Driven Approaches
Eleven studies used factor analysis and one study used cluster analysis. These analyses were all conducted using data from prospective cohort studies published between 2004 and 2012 and had sample sizes ranging from 690 to more than 75,000 individuals. Five studies were conducted in the United States and the rest from developed countries around the world. Each study identified one to four dietary patterns, with the most common comparison between "western"/"unhealthy" and "prudent"/"healthier" patterns; a total of 35 diverse dietary patterns were identified within the body of evidence. Many studies had null findings, particularly studies with duration of less than 7 years of follow up.11-14 Patterns associated with lower risk of type 2 diabetes were characterized by higher intakes of vegetables, fruits, low-fat dairy products, and whole grains, and those associated with increased risk were characterized by higher intakes of red meat, sugar-sweetened foods and drinks, French fries, refined grains, and high-fat dairy products. However, the food groups identified varied substantially, even among patterns with the same name.
Three prospective cohort studies used reduced rank regression to examine the relationship between dietary patterns and type 2 diabetes.15-17 Two of the studies were conducted in the United States and one in the United Kingdom. The sample sizes were 880 for Liese (2009), 2,879 for Imamura (2009), and 6,699 for McNaughton (2008). The independent variables in these studies were dietary pattern scores, and biomarkers were used as response variables in two of the studies. Dietary patterns that included meat intake and incident type 2 diabetes were positively associated in the two studies that used biomarkers as response variables, though the definitions of meat differed.15, 16 However, because so few studies were available and the methodology used and different populations considered varied so much, the information was insufficient to assess consistency or draw conclusions.
Other Dietary Patterns
The body of evidence examined included seven studies conducted between 2004 and 2013, consisting of six RCTs18-24 and one prospective cohort study (PCS).25 Two studies were conducted in the United States; one in the United States and Canada; one in Spain (2 PREDIMED articles); and one each in Greece, Italy, and Sweden. The sample sizes of the RCTs ranged from 82 to 1,224 participants and the PCS had a sample size of 41,387 participants. All eight studies were conducted in adults. RCT duration ranged from 6 weeks to a median of 4 years and the PCS duration was 2 years. The RCTs were primary prevention studies of at-risk participants. Baseline health status in the study participants included those with mild hypercholesterolemia, overweight or obesity, metabolic syndrome, abdominal obesity, and three or more CVD risk factors, including metabolic syndrome. The PCS participants were individuals in the Adventist Health Study who did not have type 2 diabetes.25 Three studies looked at a Mediterranean-style diet,20, 22-24 one study examined the Nordic diet (defined by the authors of the study as a diet rich in high-fiber plant foods, fruits, berries, vegetables, whole grains, rapeseed oil, nuts, fish and low-fat milk products, but low in salt, added sugars, and saturated fats),18 and three studies looked at either the DASH diet or a variation of the DASH diet,19, 21 or a vegetarian diet.25
Two of the seven studies examined the association between adherence to a dietary pattern and incidence of type 2 diabetes.24, 25 Although the results of both studies showed a favorable association between either a Mediterranean-style or a vegetarian dietary pattern and incidence of type 2 diabetes the studies differed in design and dietary pattern used to assess diet exposure. The other studies examined the intermediate outcomes of impaired glucose tolerance and/or insulin resistance and are discussed in the next section.
Dietary Patterns and Intermediate Outcomes
Five studies examined adherence to a dietary pattern and intermediate outcomes related to glucose tolerance and/or insulin resistance: two RCTs26, 27 and three prospective cohort studies.8, 9, 28 It was difficult to assess food components across these studies, as numerous different scores were used and no compelling number of studies used any one score or index. Even so, favorable associations between dietary patterns and intermediate outcomes were found.
The two RCTs were conducted in populations in Europe that were at risk of diabetes. An early report from the PREDIMED trial showed that a Mediterranean diet decreased fasting blood glucose, fasting insulin, and HOMA-IR scores in a Spanish population at risk of CVD.26 In the Oslo Diet and Exercise Study (ODES), increased adherence to the authors’ a priori diet score resulted in decreased fasting insulin and insulin after a glucose challenge, but not fasting glucose, in Norwegian men with metabolic syndrome.27 Results from prospective cohort studies were consistent in showing a favorable association between diet score and fasting glucose, fasting insulin or HOMA-IR,8, 28 with the exception of one study that found the association with fasting glucose only in men.9
Data-Driven Approaches
Variations in populations studies, definition of outcomes, dietary assessment methodologies, and methods used to derive patterns resulted in a highly variable set of dietary patterns, thus making it difficult to draw conclusions from studies using data-driven approaches. For example, one study measured fasting blood glucose with a cutoff of 6.1 and greater mmol/L;29 another study measured plasma glucose with a cutoff of 5.1 and greater mmol/L,30 while a third study measured plasma glucose after an overnight fast and after a standard 75 g oral glucose tolerance test.31 Three prospective cohort studies assessed the association between dietary patterns and plasma glucose levels. Two U.S. studies derived patterns using cluster analysis29, 30 and one study conducted in Denmark used factor analysis.31 Duffey et al. identified two diet clusters: “Prudent Diet” and “Western Diet”;29 Kimokoti et al. identified five clusters: “Heart Healthier,” “Lighter Eating,” “Wine and Moderate Eating,” “Higher Fat,” and “Empty Calories”;30 and Lau et al. derived two factors: “Modern” and “Traditional.”31
Table 1: Summary of existing reports, systematic reviews, and meta-analyses examining the relationship between dietary patterns and risk of type 2 diabetes
|
Question/ Purpose AMSTAR Rating* |
Dietary Patterns and Outcomes |
Included Studies** (Number and Study Design) |
Evidence/ Conclusion Statement from Existing Report/ SR/ MA |
|
|---|---|---|---|---|
|
NEL Dietary Patterns Systematic Review Project, 2014 |
||||
|
Overarching Finding/ Recommendation: The bodies of evidence examining the relationship between dietary patterns and risk of type 2 diabetes were limited or insufficient, but they generally supported consumption of a dietary pattern rich in fruits and vegetables and low in high-fat dairy and meats. |
||||
|
What is the relationship between adherence to dietary guidelines/ recommendations or specific dietary patterns, assessed using an index or score, and risk of type 2 diabetes? |
Dietary pattern assessed using index/score methodology Glucose intolerance, insulin resistance, incidence of T2D |
11 9 PCS; 2 RCT |
There is limited evidence that adherence to a dietary pattern rich in fruits, vegetables, legumes, cereals/whole grains, nuts, fish, and unsaturated oils, and low in meat, and high fat dairy, assessed using an index or score, is associated with decreased risk of type 2 diabetes. (Limited) |
|
|
Are prevailing patterns of dietary intake in a population, derived using cluster or factor analysis, related to the risk of type 2 diabetes? |
Dietary pattern assessed using factor or cluster analysis Glucose intolerance, insulin resistance, incidence of T2D |
15 15 PCS |
Limited and inconsistent evidence from epidemiological studies indicates that in adults, dietary patterns derived using factor or cluster analysis, characterized by vegetables, fruits, and low-fat dairy products tend to have an association with decreased risk of type 2 diabetes and those patterns characterized by red meat, sugar-sweetened foods and drinks, French fries, refined grains and high-fat dairy products tended to show an increased association for risk of type 2 diabetes. Among studies there was substantial variation in food group components and not all studies with similar patterns showed significant association. (Limited) |
|
|
What combinations of food intake, assessed using reduced rank regression, explain the most variation in risk of type 2 diabetes? |
Dietary pattern assessed using reduced rank regression Glucose intolerance, insulin resistance, incidence of T2D |
3 3 PCS |
There is insufficient evidence, due to a small number of studies, to examine the relationship between dietary patterns derived using reduced rank regression and risk of type 2 diabetes. The differences in the methods used and populations studied made it difficult to compare results, and therefore no conclusions were drawn. (Grade not Assignable) |
|
|
What is the relationship between adherence to dietary guidelines/ recommendations or specific dietary patterns, assessed using methods other than index/score, cluster or factor, or reduced rank regression analyses, and risk of type 2 diabetes? |
Dietary pattern assessed using methodologies other than index, factor, cluster, or reduced rank regression analyses Glucose intolerance, insulin resistance, incidence of T2D |
8 7 RCT (from 6 trials); 1 PCS |
There is insufficient evidence on a relationship between adherence to a Mediterranean-style or vegetarian diet pattern and incidence of type 2 diabetes. There is limited, inconsistent evidence that adherence to a Mediterranean-style, DASH or modified DASH, or Nordic dietary pattern results in improved glucose tolerance and insulin resistance. (Limited – Intermediate outcomes; Grade not Assignable – T2D incidence) |
|
|
Alhazmi, 2013 |
||||
|
Association between dietary patterns and risk of type 2 diabetes Meta-analysis AMSTAR: 11/11 |
"Healthy" and "unhealthy" dietary patterns; for studies that reported more than one dietary pattern, only the patterns that shared similar characteristics with the healthy/unhealthy pattern were included in the meta-analysis Incidence of T2D |
15 15 PCS |
The results of this systematic review and meta-analysis indicate that dietary patterns may be associated with the risk of type 2 diabetes. There was evidence of a reduction in the risk of type 2 diabetes in the highest adherence compared to the lowest adherence to healthy dietary patterns [RR = 0.79, 95% confidence interval (CI): 0.74 to 0.86, P < 0.005]. An increase in the risk of type 2 diabetes was evident for the highest adherence compared to the lowest adherence to unhealthy dietary patterns (RR = 1.44, 95% CI: 1.33 to 1.57, P < 0.005). The results indicated that dietary patterns consisting of healthy foods and/or nutrient choices and had higher energy contributions from whole grain products, fruit and vegetables may decrease the risk of type 2 diabetes. By contrast, dietary patterns represented by unhealthy food choices and higher energy contributions from foods such as red or processed meats, high-fat dairy, refined grains and sweets may increase the risk of developing type 2 diabetes. |
|
*A measurement tool for the ‘assessment of multiple systematic reviews’ (AMSTAR)
** Reference overlap: Of the 39 articles included in total across the reviews, 13 were included in both reviews.
References Included in Review
- Nutrition Evidence Library. A series of systematic reviews on the relationship between dietary patterns and health outcomes. Alexandria, VA: U.S. Department of Agriculture, Center for Nutrition Policy and Promotion, March 2014. Available from: http://www.nel.gov/vault/2440/web/files/DietaryPatterns/DPRptFullFinal.pdf [PDF - 6.1 MB].
- Alhazmi A, Stojanovski E, McEvoy M, Garg ML. The association between dietary patterns and type 2 diabetes: a systematic review and meta-analysis of cohort studies. J Hum Nutr Diet. 2014 Jun;27(3):251-60. PMID: 24102939.http://www.ncbi.nlm.nih.gov/pubmed/24102939.
Additional References
- Liese AD, Nichols M, Sun X, D'Agostino RB, Haffner SM. Adherence to the DASH Diet is inversely associated with incidence of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes Care. 2009;32(8):1434-6. PMID: 19487638. http://www.ncbi.nlm.nih.gov/pubmed/19487638.
- Martínez-González MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z, et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ. 2008;336(7657):1348-51. PMID: 18511765. http://www.ncbi.nlm.nih.gov/pubmed/18511765.
- Rossi M, Turati F, Lagiou P, Trichopoulos D, Augustin LS, La Vecchia C, et al. Mediterranean diet and glycaemic load in relation to incidence of type 2 diabetes: results from the Greek cohort of the population-based European Prospective Investigation into Cancer and Nutrition (EPIC). Diabetologia. 2013;56(11):2405-13. PMID: 23975324. http://www.ncbi.nlm.nih.gov/pubmed/23975324.
- Abiemo EE, Alonso A, Nettleton JA, Steffen LM, Bertoni AG, Jain A, et al. Relationships of the Mediterranean dietary pattern with insulin resistance and diabetes incidence in the Multi-Ethnic Study of Atherosclerosis (MESA). Br J Nutr. 2013;109(8):1490-7. PMID: 22932232. http://www.ncbi.nlm.nih.gov/pubmed/22932232.
- Fung TT, McCullough M, van Dam RM, Hu FB. A prospective study of overall diet quality and risk of type 2 diabetes in women. Diabetes Care. 2007;30(7):1753-7. PMID: 17429059. http://www.ncbi.nlm.nih.gov/pubmed/17429059.
- Zamora D, Gordon-Larsen P, He K, Jacobs DR, Shikany JM, Popkin BM. Are the 2005 Dietary Guidelines for Americans Associated With reduced risk of type 2 diabetes and cardiometabolic risk factors? Twenty-year findings from the CARDIA study. Diabetes Care. 2011;34(5):1183-5. PMID: 21478463. http://www.ncbi.nlm.nih.gov/pubmed/21478463.
- Gopinath B, Rochtchina E, Flood VM, Mitchell P. Diet quality is prospectively associated with incident impaired fasting glucose in older adults. Diabet Med. 2013;30(5):557-62. PMID: 23301551. http://www.ncbi.nlm.nih.gov/pubmed/23301551.
- von Ruesten A, Illner AK, Buijsse B, Heidemann C, Boeing H. Adherence to recommendations of the German food pyramid and risk of chronic diseases: results from the EPIC-Potsdam study. Eur J Clin Nutr. 2010;64(11):1251-9. PMID: 20717136. http://www.ncbi.nlm.nih.gov/pubmed/20717136.
- Malik VS, Fung TT, van Dam RM, Rimm EB, Rosner B, Hu FB. Dietary patterns during adolescence and risk of type 2 diabetes in middle-aged women. Diabetes Care. 2012;35(1):12-8. PMID: 22074723. http://www.ncbi.nlm.nih.gov/pubmed/22074723.
- Hodge AM, English DR, O'Dea K, Giles GG. Dietary patterns and diabetes incidence in the Melbourne Collaborative Cohort Study. Am J Epidemiol. 2007;165(6):603-10. PMID: 17220476. http://www.ncbi.nlm.nih.gov/pubmed/17220476.
- Nanri A, Shimazu T, Takachi R, Ishihara J, Mizoue T, Noda M, et al. Dietary patterns and type 2 diabetes in Japanese men and women: the Japan Public Health Center-based Prospective Study. Eur J Clin Nutr. 2013;67(1):18-24. PMID: 23093343. http://www.ncbi.nlm.nih.gov/pubmed/23093343.
- Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR. Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2008;31(9):1777-82. PMID: 18544792. http://www.ncbi.nlm.nih.gov/pubmed/18544792.
- Liese AD, Weis KE, Schulz M, Tooze JA. Food intake patterns associated with incident type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2009;32(2):263-8. PMID: 19033409. http://www.ncbi.nlm.nih.gov/pubmed/19033409.
- McNaughton SA, Mishra GD, Brunner EJ. Dietary patterns, insulin resistance, and incidence of type 2 diabetes in the Whitehall II Study. Diabetes Care. 2008;31(7):1343-8. PMID: 18390803. http://www.ncbi.nlm.nih.gov/pubmed/18390803.
- Imamura F, Lichtenstein AH, Dallal GE, Meigs JB, Jacques PF. Generalizability of dietary patterns associated with incidence of type 2 diabetes mellitus. Am J Clin Nutr. 2009;90(4):1075-83. PMID: 19710193. http://www.ncbi.nlm.nih.gov/pubmed/19710193.
- Adamsson V, Reumark A, Fredriksson IB, Hammarström E, Vessby B, Johansson G, et al. Effects of a healthy Nordic diet on cardiovascular risk factors in hypercholesterolaemic subjects: a randomized controlled trial (NORDIET). J Intern Med. 2011;269(2):150-9. PMID: 20964740. http://www.ncbi.nlm.nih.gov/pubmed/20964740.
- Blumenthal JA, Babyak MA, Sherwood A, Craighead L, Lin PH, Johnson J, et al. Effects of the dietary approaches to stop hypertension diet alone and in combination with exercise and caloric restriction on insulin sensitivity and lipids. Hypertension. 2010;55(5):1199-205. PMID: 20212264. http://www.ncbi.nlm.nih.gov/pubmed/20212264.
- Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, et al. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004;292(12):1440-6. PMID: 15383514. http://www.ncbi.nlm.nih.gov/pubmed/15383514.
- Gadgil MD, Appel LJ, Yeung E, Anderson CA, Sacks FM, Miller ER. The effects of carbohydrate, unsaturated fat, and protein intake on measures of insulin sensitivity: results from the OmniHeart trial. Diabetes Care. 2013;36(5):1132-7. PMID: 23223345. http://www.ncbi.nlm.nih.gov/pubmed/23223345.
- Rallidis LS, Lekakis J, Kolomvotsou A, Zampelas A, Vamvakou G, Efstathiou S, et al. Close adherence to a Mediterranean diet improves endothelial function in subjects with abdominal obesity. Am J Clin Nutr. 2009;90(2):263-8. PMID: 19515732. http://www.ncbi.nlm.nih.gov/pubmed/19515732.
- Salas-Salvadó J, Fernández-Ballart J, Ros E, Martínez-González MA, Fitó M, Estruch R, et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: one-year results of the PREDIMED randomized trial. Arch Intern Med. 2008;168(22):2449-58. PMID: 19064829. http://www.ncbi.nlm.nih.gov/pubmed/19064829.
- Salas-Salvadó J, Bulló M, Babio N, Martínez-González M, Ibarrola-Jurado N, Basora J, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011;34(1):14-9. PMID: 20929998. http://www.ncbi.nlm.nih.gov/pubmed/20929998.
- Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis. 2013;23(4):292-9. PMID: 21983060. http://www.ncbi.nlm.nih.gov/pubmed/21983060.
- Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145(1):1-11. PMID: 16818923. http://www.ncbi.nlm.nih.gov/pubmed/16818923.
- Jacobs DR, Sluik D, Rokling-Andersen MH, Anderssen SA, Drevon CA. Association of 1-y changes in diet pattern with cardiovascular disease risk factors and adipokines: results from the 1-y randomized Oslo Diet and Exercise Study. Am J Clin Nutr. 2009;89(2):509-17. PMID: 19116328. http://www.ncbi.nlm.nih.gov/pubmed/19116328.
- Rumawas ME, Meigs JB, Dwyer JT, McKeown NM, Jacques PF. Mediterranean-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the Framingham Offspring Cohort. Am J Clin Nutr. 2009;90(6):1608-14. PMID: 19828705. http://www.ncbi.nlm.nih.gov/pubmed/19828705.
- Duffey KJ, Steffen LM, Van Horn L, Jacobs DR, Popkin BM. Dietary patterns matter: diet beverages and cardiometabolic risks in the longitudinal Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr. 2012;95(4):909-15. PMID: 22378729. http://www.ncbi.nlm.nih.gov/pubmed/22378729.
- Kimokoti RW, Gona P, Zhu L, Newby PK, Millen BE, Brown LS, et al. Dietary patterns of women are associated with incident abdominal obesity but not metabolic syndrome. J Nutr. 2012;142(9):1720-7. PMID: 22833658. http://www.ncbi.nlm.nih.gov/pubmed/22833658.
- Lau C, Toft U, Tetens I, Carstensen B, Jørgensen T, Pedersen O, et al. Dietary patterns predict changes in two-hour post-oral glucose tolerance test plasma glucose concentrations in middle-aged adults. J Nutr. 2009;139(3):588-93. PMID: 19158222. http://www.ncbi.nlm.nih.gov/pubmed/19158222.
- National Heart, Lung, and Blood Institute. Lifestyle Interventions to Reduce Cardiovascular Risk: Systematic Evidence Review from the Lifestyle Work Group, 2013. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, 2013. Available from: http://www.nhlbi.nih.gov/guidelines/cvd_adult/lifestyle/index.htm
Associated Lifestyle Guideline:
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2960-84. PMID: 24239922. http://www.ncbi.nlm.nih.gov/pubmed/24239922
- National Heart Lung and Blood Institute. Managing overweight and obesity in adults: Systematic evidence review from the Obesity Expert Panel, 2013. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health; 2013. Available from: http://www.nhlbi.nih.gov/guidelines/obesity/ser/index.htm.
Associated Guideline
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985-3023. PMID: 24239920. http://www.ncbi.nlm.nih.gov/pubmed/24239920.
Supplementary Information:
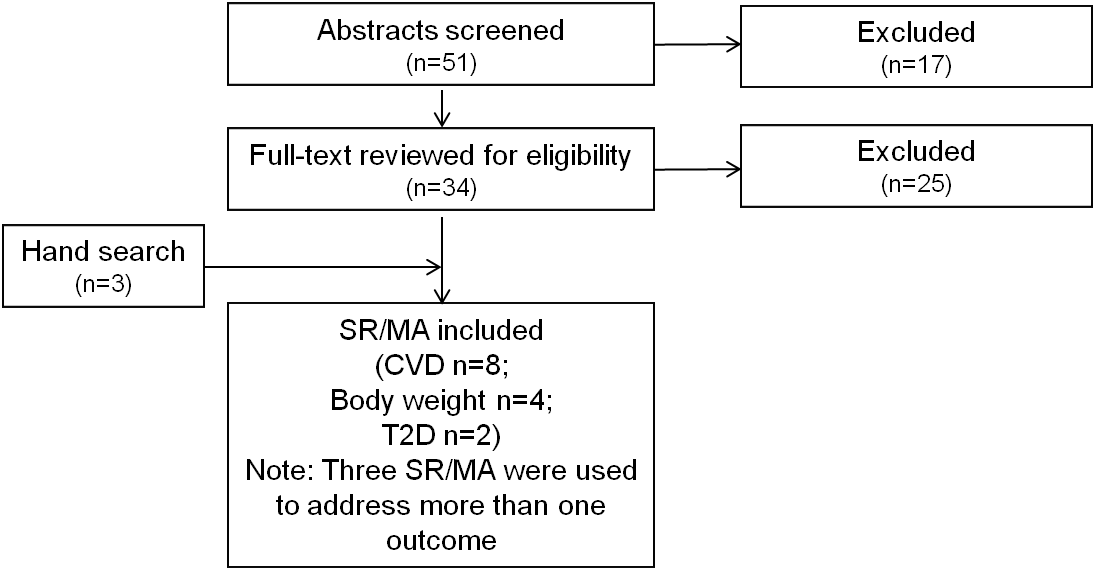
(Note: The search and update for the dietary patterns and CVD, body weight, and type 2 diabetes reviews were done simultaneously and are described together below.)
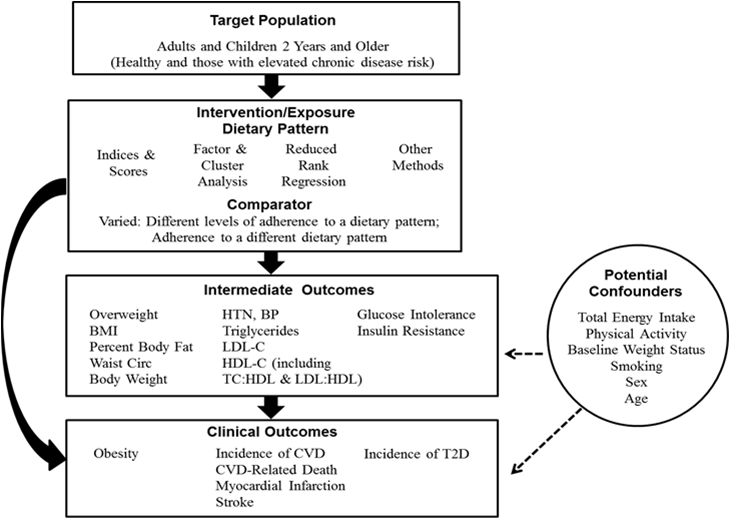
Analytical Framework
Methodology
The questions examining dietary patterns and risk of CVD, obesity, and type 2 diabetes were answered using existing reports, systematic reviews, and meta-analyses. All three of these questions were addressed in the Nutrition Evidence Library (NEL) Dietary Patterns Systematic Review Project. This project was supported by USDA’s Center for Nutrition Policy and Promotion and was informed by a Technical Expert Collaborative of experts in dietary patterns research.1 Additionally, the DGAC reviewed reports from systematic reviews recently conducted by the National Heart, Lung, and Blood Institute (NHLBI) that included dietary patterns research. For CVD, the DGAC used the NHLBI Lifestyle Interventions to Reduce Cardiovascular Risk: Systematic Evidence Review from the Lifestyle Work Group and the associated American Heart Association (AHA)/ American College of Cardiology (ACC) Guideline on Lifestyle Management to Reduce Cardiovascular Risk.32 For body weight, the DGAC used the NHLBI Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel and the associated AHA/ACC/ The Obesity Society (TOS)Guideline for the Management of Overweight and Obesity in Adults.33 For all three questions, in an attempt to capture new research published since the searches for these systematic reviews were completed, the Committee considered existing systematic reviews and meta-analyses published in peer-reviewed journals since 2008. The existing systematic reviews and meta-analyses considered by the DGAC had to meet the general inclusion criteria of the DGAC, and were required to consider dietary patterns and the outcomes of interest.
Search Strategy for Existing Systematic Reviews/Meta-Analyses
(“diet quality” OR dietary pattern* OR diet pattern* OR eating pattern* OR food pattern* OR eating habit* OR dietary habit* OR food habit* OR dietary profile* OR food profile* OR diet profile* OR eating profile* OR dietary guideline* OR dietary recommendation* OR food intake pattern* OR dietary intake pattern* OR diet pattern* OR eating style*) OR
(DASH OR (dietary approaches to stop hypertension) OR "Diet, Mediterranean"[Mesh] OR vegan* OR vegetarian* OR "Diet, Vegetarian"[Mesh] OR “prudent diet” OR “western diet” OR nordiet OR omniheart OR (Optimal Macronutrient Intake Trial to Prevent Heart Disease) OR ((Okinawa* OR "Ethnic Groups"[Mesh] OR “plant based” OR Mediterranean[tiab]OR Nordic) AND (diet[mh] OR diet[tiab] OR food[mh])))
OR
("Guideline Adherence"[Mesh] AND (diet OR food OR eating OR eat OR dietary OR feeding OR nutrition OR nutrient*)) OR (adherence AND (nutrient* OR nutrition OR diet OR dietary OR food OR eat OR eating) AND (guideline* OR guidance OR recommendation*)) OR
(dietary score* OR adequacy index* OR kidmed OR Diet Quality Index* OR Food Score* OR Diet Score* OR MedDietScore OR Dietary Pattern Score* OR “healthy eating index”)OR
((index*[ti] OR score*[ti] OR indexes OR scoring[ti] indices[ti]) AND (dietary[ti] OR nutrient*[ti] OR eating[tiab] OR OR food[ti] OR food[mh] OR diet[ti] OR diet[mh]) AND (pattern* OR habit* OR profile*))
Body weight:
("body size"[tiab] OR body size[mh] OR obesity[tiab] OR obese[tiab] OR obesity[mh] OR overweight [tiab] OR adiposity[tiab] OR adiposity[mh] OR "body weight"[tiab] OR body weight[mh] OR “body-weight related”[tiab] OR "weight gain"[tiab] OR weight gain[mh] OR "weight loss"[tiab] OR Body Weights and Measures[Majr] OR overweight[tiab] OR "Body Composition"[mh] OR "body fat"[tiab] OR adipos*[tiab] OR weight[ti] OR waist[ti] OR "Anthropometry"[Mesh:noexp] OR “body mass index”[tiab] OR BMI[tiab] OR “weight status”[tiab] OR adipose tissue [mh] OR "healthy weight"[tiab] OR waist circumference[mh] OR “body fat mass”[tiab] OR body weight changes[mh] OR “waist circumference”[tiab])
CVD:
"Mortality"[Mesh] OR mortality[tiab] OR "blood pressure"[tiab] OR "blood pressure"[mesh] OR "cardiovascular diseases"[mh:noexp] OR cardiovascular disease*[tiab] OR cardiovascular event*[tiab] OR "cholesterol/blood"[mh] OR "Cholesterol, HDL"[Mesh] OR cholesterol[tiab] OR "Cholesterol, Dietary"[Mesh] OR triglyceride* OR stroke[tiab] OR "stroke"[Mesh] OR "Lipids/blood"[Mesh] OR hypertension[tiab] OR "Myocardial Infarction"[Mesh] OR "Myocardial Infarction"[tiab] OR "Heart Failure"[Mesh] OR "Heart Arrest"[Mesh] OR "Myocardial Ischemia"[Mesh] OR "heart failure"[tiab] OR "heart arrest"[tiab] OR "Myocardial Ischemia"[tiab] OR hypertension[mh]
T2D:
(“insulin resistance”[mh] OR “insulin”[ti] OR inflammation[ti] OR glucose intoleran*[ti] OR "Glucose Intolerance"[Mesh] OR diabetes[ti] OR "Diabetes Mellitus, Type 2"[Mesh] OR "Hemoglobin A, Glycosylated"[Mesh] OR “hemoglobin A1c “[ti] OR (“impaired fasting” AND (glucose OR glycemi*)) OR “onset diabetes” OR “impaired glucose” OR “insulin sensitivity”)
AND limit to: systematic[sb] OR systematic review* OR meta-analys* OR meta analys*
Inclusion Criteria
Date Range:
- Published between January 2008 and April 2014 (in English in a peer-reviewed journal)
Study Design:
- Systematic review and/or meta-analysis that included randomized controlled trials and/or prospective cohort studies
Study Subjects:
- Reviews that included studies from high or very high human development (2012 Human Development Index)
- Healthy or at elevated chronic disease risk
Intervention/Exposure:
- Dietary pattern - The quantities, proportions, variety, or combination of different foods, drinks, and nutrients (when available) in diets, and the frequency with which they are habitually consumed.
Outcome:
- CVD: LDL-cholesterol, HDL-cholesterol, triglycerides, blood pressure, incidence of CVD, CVD-related death, myocardial infarction, or stroke
- Body weight: Body mass index, body weight, percent body fat, waist circumference, incidence of overweight or obesity
- Type 2 diabetes: Glucose intolerance, insulin resistance, or incidence of type 2 diabetes
Quality:
- Reviews rated 8-11 on AMSTAR (A measurement tool for the ‘assessment of multiple systematic reviews’)
Search Results
Excluded Articles with Reason for Exclusion
- Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013 Mar;97(3):505-16. doi: 10.3945/ajcn.112.042457. Epub 2013 Jan 30. Review. PubMed PMID: 23364002. EXCLUDE: Examined subjects diagnosed with type 2 diabetes (management of type 2 diabetes)
- Akesson A, Andersen LF, Kristjánsdóttir AG, Roos E, Trolle E, Voutilainen E, Wirfält E. Health effects associated with foods characteristic of the Nordic diet: a systematic literature review. Food Nutr Res. 2013;57. doi: 10.3402/fnr.v57i0.22790. Review. PubMed PMID: 24130513; PubMed Central PMCID: PMC3795297. EXCLUDE: Examined individual components of the diet, not dietary patterns as defined by the Subcommittee
- Aljadani H., Patterson A., Sibbritt D., Collins C. The association between dietary patterns and weight change in adults over time: A systematic review of studies with follow up. JBI Database of Systematic Reviews and Implementation Reports 2013 11:8 (272-316) EXCLUDE: Did not examine dietary patterns as defined by the Subcommittee
- Al-Khudairy L, Stranges S, Kumar S, Al-Daghri N, Rees K. Dietary factors and type 2 diabetes in the Middle East: what is the evidence for an association?--a systematic review. Nutrients. 2013 Sep 26;5(10):3871-97. doi: 10.3390/nu5103871. PubMed PMID: 24077241; PubMed Central PMCID: PMC3820049. EXCLUDE: Not all countries in the Middle East are of high or very high development according to the Human Development Index
- Barbaresko J, Koch M, Schulze MB, Nöthlings U. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev. 2013 Aug;71(8):511-27. doi: 10.1111/nure.12035. Epub 2013 Jun 13. Review. PubMed PMID: 23865797. EXCLUDE: Outcomes were inflammatory markers, which were not included as intermediate outcomes in the Subcommittee’s analytical framework
- Buckland G, Bach A, Serra-Majem L. Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev. 2008 Nov;9(6):582-93. doi: 10.1111/j.1467-789X.2008.00503.x. Epub 2008 Jun 10. Review. PubMed PMID: 18547378 EXCLUDE: AMSTAR rating was 7 of 11
- Carter P, Achana F, Troughton J, Gray LJ, Khunti K, Davies MJ. A Mediterranean diet improves HbA1c but not fasting blood glucose compared to alternative dietary strategies: a network meta-analysis. J Hum Nutr Diet. 2013 Jun 22. doi: 10.1111/jhn.12138. [Epub ahead of print] PubMed PMID: 23790149. EXCLUDE: Half of the studies included in the meta-analyses only included participants with T2D or CVD
- Chan M.Y., Yulianna Y. Effect of mediterranean diet components on selected cardiovascular risk factors, all-cause mortality and cardiovascular mortality: Systematic review. Annals of Nutrition and Metabolism 2013 63 SUPPL. 1 (1093) EXCLUDE: Abstract, not a full article
- Defagó M., Elorriaga N., Irazola V., Rubinstein A.Association between food patterns and biomarkers of endothelial function: A systematic review. Annals of Nutrition and Metabolism 2013 63 SUPPL. 1 (1282) EXCLUDE: Outcomes were biomarkers of endothelial function, which were not included as intermediate outcomes in the Subcommittee’s analytical framework
- Dong JY, Zhang ZL, Wang PY, Qin LQ. Effects of high-protein diets on body weight, glycaemic control, blood lipids and blood pressure in type 2 diabetes: meta-analysis of randomised controlled trials. Br J Nutr. 2013 Sep 14;110(5):781-9. doi: 10.1017/S0007114513002055. Epub 2013 Jul 5. Review. PubMed PMID: 23829939. EXCLUDE: Participants were diagnosed with type 2 diabetes
- Esposito K, Kastorini CM, Panagiotakos DB, Giugliano D. Mediterranean diet and metabolic syndrome: an updated systematic review. Rev Endocr Metab Disord. 2013 Sep;14(3):255-63. doi: 10.1007/s11154-013-9253-9. PubMed PMID: 23982678. EXCLUDE: Included cross-sectional studies; examined incidence of metabolic syndrome, which is outside the scope of the Subcommittee’s analytical framework
- Esposito K, Kastorini CM, Panagiotakos DB, Giugliano D. Prevention of type 2 diabetes by dietary patterns: a systematic review of prospective studies and meta-analysis. Metab Syndr Relat Disord. 2010 Dec;8(6):471-6. doi: 10.1089/met.2010.0009. Epub 2010 Oct 19. Review. PubMed PMID: 20958207.EXCLUDE: Of the 10 included studies, 8 were included in the NEL and Alhamzi reviews being considered by the Committee
- Esposito K, Maiorino MI, Ceriello A, Giugliano D. Prevention and control of type 2 diabetes by Mediterranean diet: a systematic review. Diabetes Res Clin Pract. 2010 Aug;89(2):97-102. doi: 10.1016/j.diabres.2010.04.019. Epub 2010 May 23. Review. PubMed PMID: 20546959. EXCLUDE: Only 3 studies looked at prevention and one was cross-sectional
- Grosso G, Mistretta A, Frigiola A, Gruttadauria S, Biondi A, Basile F, Vitaglione P, D'Orazio N, Galvano F. Mediterranean diet and cardiovascular risk factors: a systematic review. Crit Rev Food Sci Nutr. 2014;54(5):593-610. doi: 10.1080/10408398.2011.596955. PubMed PMID: 24261534. EXCLUDE: Included cross-sectional studies; included various outcomes not included in the Subcommittee’s analytical framework, including incidence of metabolic syndrome, CRP, IL-6, liver transaminases, etc.
- Hu T, Mills KT, Yao L, Demanelis K, Eloustaz M, Yancy WS Jr, Kelly TN, He J, Bazzano LA. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Am J Epidemiol. 2012 Oct 1;176 Suppl 7:S44-54. doi: 10.1093/aje/kws264. PubMed PMID: 23035144; PubMed Central PMCID: PMC3530364. EXCLUDE: Did not examine dietary patterns as described by the Subcommittee
- Joung H, Hong S, Song Y, Ahn BC, Park MJ. Dietary patterns and metabolic syndrome risk factors among adolescents. Korean J Pediatr. 2012 Apr;55(4):128-35. doi: 10.3345/kjp.2012.55.4.128. Epub 2012 Apr 30. PubMed PMID: 22574073; PubMed Central PMCID: PMC3346835. EXCLUDE: Meta-analysis of cross-sectional data
- Kant AK. Dietary patterns: biomarkers and chronic disease risk. Appl Physiol Nutr Metab. 2010 Apr;35(2):199-206. doi: 10.1139/H10-005. Review. PubMed PMID: 20383233. EXCLUDE: Narrative review
- Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011 Mar 15;57(11):1299-313. doi: 10.1016/j.jacc.2010.09.073. PubMed PMID: 21392646.EXCLUDE: Included cross-sectional studies
- Kastorini CM, Milionis HJ, Goudevenos JA, Panagiotakos DB. Mediterranean diet and coronary heart disease: is obesity a link? - A systematic review. Nutr Metab Cardiovasc Dis. 2010 Sep;20(7):536-51. doi: 10.1016/j.numecd.2010.04.006. Review. PubMed PMID: 20708148. EXCLUDE: Included cross-sectional studies and secondary prevention studies
- Kastorini CM, Panagiotakos DB. Dietary patterns and prevention of type 2 diabetes: from research to clinical practice; a systematic review. Curr Diabetes Rev. 2009 Nov;5(4):221-7. Review. PubMed PMID: 19531025.EXCLUDE: Included cross-sectional and case-control studies
- Kwan MW, Wong MC, Wang HH, Liu KQ, Lee CL, Yan BP, Yu CM, Griffiths SM. Compliance with the Dietary Approaches to Stop Hypertension (DASH) diet: a systematic review. PLoS One. 2013;8(10):e78412. doi: 10.1371/journal.pone.0078412. PubMed PMID: 24205227; PubMed Central PMCID: PMC3813594. EXCLUDE: Examined compliance to the DASH diet
- Maghsoudi Z, Azadbakht L. How dietary patterns could have a role in prevention, progression, or management of diabetes mellitus? Review on the current evidence. J Res Med Sci. 2012 Jul;17(7):694-709. PubMed PMID: 23798934; PubMed Central PMCID: PMC3685790. EXCLUDE: Included cross-sectional studies and seminars and symposiums
- Marshall S, Burrows T, Collins CE. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J Hum Nutr Diet. 2014 Feb 13. doi: 10.1111/jhn.12208. [Epub ahead of print] PubMed PMID: 24524271. EXCLUDE: Included cross-sectional and case-control studies; included abstracts; focus of review was to describe indices being used with children and adolescents – only brief mention of body weight and no conclusions drawn.
- Martínez-González MÁ, Martín-Calvo N. The major European dietary patterns and metabolic syndrome. Rev Endocr Metab Disord. 2013 Sep;14(3):265-71. doi: 10.1007/s11154-013-9264-6. PubMed PMID: 23979531. EXCLUDE: Narrative review
- McEvoy C., Cardwell C., Woodside J., Young I., Hunter S., McKinley M. A systematic review and meta-analysis examining 'a posteriori' dietary patterns and risk of type 2 diabetes. Annals of Nutrition and Metabolism 2013 63 SUPPL. 1 (864) EXCLUDE: Abstract, not a full article
- Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009 Apr 13;169(7):659-69. doi:10.1001/archinternmed.2009.38. Review. PubMed PMID: 19364995. EXCLUDE: Some studies included secondary prevention, did not provide list of included articles; describes dietary factors, rather than dietary pattern as defined by the SC
- Nordmann A.J., Suter K., Tuttle K.R., Estruch R., Shai I., Bucher H. Meta-analysis of Mediterranean versus low-fat diets to improve cardiovascular risk factors. European Heart Journal 2010 31 SUPPL. 1 (940) EXCLUDE: Abstract, not a full article
- Osei-Assibey G, Boachie C. Dietary interventions for weight loss and cardiovascular risk reduction in people of African ancestry (blacks): a systematic review. Public Health Nutr. 2012 Jan;15(1):110-5. doi: 10.1017/S1368980011001121. Epub 2011 Jun 1. Review. PubMed PMID: 21729478. EXCLUDE: Examined dietary interventions, in general, not dietary patterns specifically
- Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann Neurol. 2013 Oct;74(4):580-91. doi: 10.1002/ana.23944. Epub 2013 Sep 16. PubMed PMID: 23720230. EXCLUDE: Included case-control studies
- Santos FL, Esteves SS, da Costa Pereira A, Yancy WS Jr, Nunes JP. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev. 2012 Nov;13(11):1048-66. doi: 10.1111/j.1467-789X.2012.01021.x. Epub 2012 Aug 21. Review. PubMed PMID: 22905670. EXCLUDE: Did not examine dietary patterns as described by the SC
- Schwingshackl L, Hoffmann G. Long-term effects of low-fat diets either low or high in protein on cardiovascular and metabolic risk factors: a systematic review and meta-analysis. Nutr J. 2013 Apr 15;12:48. doi: 10.1186/1475-2891-12-48. Review. PubMed PMID: 23587198; PubMed Central PMCID: PMC3636027. EXCLUDE: Did not examine dietary patterns as described by the SC
- Shirani F, Salehi-Abargouei A, Azadbakht L. Effects of Dietary Approaches to Stop Hypertension (DASH) diet on some risk for developing type 2 diabetes: a systematic review and meta-analysis on controlled clinical trials. Nutrition. 2013 Jul-Aug;29(7-8):939-47. doi: 10.1016/j.nut.2012.12.021. Epub 2013 Mar 6. Review. PubMed PMID: 23473733.EXCLUDE: Review included articles with less than 30 participants per study arm
- Smithers LG, Golley RK, Brazionis L, Lynch JW. Characterizing whole diets of young children from developed countries and the association between diet and health: a systematic review. Nutr Rev. 2011 Aug;69(8):449-67. doi: 10.1111/j.1753-4887.2011.00407.x. Review. PubMed PMID: 21790612. EXCLUDE: Included cross-sectional studies; focus of the review was to describe what is currently known about measures of dietary patterns in early life and the general association between dietary patterns and child health and development – only brief mention of body weight
- Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010 Nov;92(5):1189-96. doi: 10.3945/ajcn.2010.29673. Epub 2010 Sep 1. Review. PubMed PMID: 20810976. EXCLUDE: Meta-analysis captured in Sofi 2013
- Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008 Sep 11;337:a1344. doi: 10.1136/bmj.a1344. Review. PubMed PMID: 18786971; PubMed Central PMCID: PMC2533524. EXCLUDE: Meta-analysis captured in Sofi 2013
- Sofi F. The Mediterranean diet revisited: evidence of its effectiveness grows. Curr Opin Cardiol. 2009 Sep;24(5):442-6. doi: 10.1097/HCO.0b013e32832f056e. Review. PubMed PMID: 19550306. EXCLUDE: Narrative review
- Summerbell CD, Douthwaite W, Whittaker V, Ells LJ, Hillier F, Smith S, Kelly S, Edmunds LD, Macdonald I. The association between diet and physical activity and subsequent excess weight gain and obesity assessed at 5 years of age or older: a systematic review of the epidemiological evidence. Int J Obes (Lond). 2009 Jul;33 Suppl 3:S1-92. doi: 10.1038/ijo.2009.80. Review. Erratum in: Int J Obes (Lond). 2010 Apr;34(4):789. abstract no. 5.3 only. Int J Obes (Lond). 2010 Apr;34(4):788. abstract no. 5.2 only. PubMed PMID: 19597430. EXCLUDE: Considered various aspects of eating, including fast food intake, frequency of eating, night eating, individual food groups, as well as physical activity, etc.; included relevant section with 6 studies, 1 considered glycemic index/load, and 4 included in NEL review
- Tyrovolas S, Panagiotakos DB. The role of Mediterranean type of diet on the development of cancer and cardiovascular disease, in the elderly: a systematic review. Maturitas. 2010 Feb;65(2):122-30. doi: 10.1016/j.maturitas.2009.07.003. Epub 2009 Aug 4. Review. PubMed PMID: 19656644. EXCLUDE: Narrative review; considers cross-sectional and case-control studies
- Vadiveloo M, Dixon LB, Parekh N. Associations between dietary variety and measures of body adiposity: a systematic review of epidemiological studies. Br J Nutr. 2013 May;109(9):1557-72. doi: 10.1017/S0007114512006150. Epub 2013 Feb 27. Review. PubMed PMID: 23445540. EXCLUDE: Examined dietary variety, not dietary patterns
- Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett J, Yancy WS Jr. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care. 2012 Feb;35(2):434-45. doi: 10.2337/dc11-2216. Review. PubMed PMID: 22275443; PubMed Central PMCID: PMC3263899. EXCLUDE: Only included studies with people with type 2 diabetes
- Yuliana Y., Chan M.Y. Effect of mediterranean diet components on selected cardiovascular risk factors, all-cause mortality and cardiovascular mortality: Systematic review. Annals of Nutrition and Metabolism 2013 63 SUPPL. 1 (981) EXCLUDE: Abstract, not a full article
- Zhang Z, Wang J, Chen S, Wei Z, Li Z, Zhao S, Lu W. Comparison of Vegetarian Diets and Omnivorous Diets on Plasma Level of HDL-c: A Meta-Analysis. PLoS One. 2014 Mar 26;9(3):e92609. doi: 10.1371/journal.pone.0092609. eCollection 2014.PubMed PMID: 24671216. EXCLUDE: Included cross-sectional studies in meta-analysis